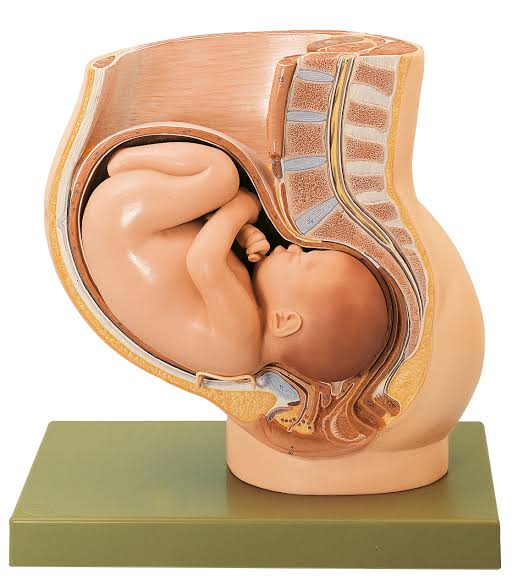
A birth canal delivery, also known as a vaginal birth, is a natural process where a baby is delivered through the mother’s vagina. It’s the most common method of childbirth.
Vaginal delivery can have various effects, both short-term and long-term, on both the mother and the baby:
For the Mother:
Short-term discomfort and recovery: After a vaginal delivery, the mother may experience soreness, swelling, and possible tearing or episiotomy (a surgical cut made at the opening of the vagina) which requires stitches. Recovery time varies, but most women start to feel better within a few weeks.
Bonding: Some mothers report feeling an immediate strong bond with their baby after a vaginal delivery due to the shared experience.
Less risk of surgical complications: Compared to a cesarean section (C-section), a vaginal delivery generally involves fewer surgical risks and a shorter hospital stay.
Potential for postpartum urinary incontinence: Some women may experience temporary urinary incontinence (leakage of urine) after vaginal delivery due to pressure on the bladder during childbirth.
Possible future pelvic floor issues: There’s a potential for pelvic floor disorders, like pelvic organ prolapse or urinary incontinence, later in life. However, these risks can often be mitigated with proper postpartum care and exercises.
For the Baby:
Beneficial bacteria exposure: Babies born vaginally are exposed to beneficial bacteria in the birth canal which can help kickstart their immune system and establish a healthy gut microbiome.
Less respiratory issues: Babies born through vaginal delivery tend to have fewer respiratory problems compared to those born via C-section.
A-Z Knowledge About Procedure Incision And Medical Care
Shaped head: The process of passing through the birth canal can temporarily mold a baby’s head, which usually resolves in a few days.
Potential for birth injuries: While rare, there’s a small risk of birth injuries like brachial plexus injuries or fractures during a vaginal delivery.
After a vaginal delivery, it’s crucial to prioritize self-care to aid in your recovery. Here are some general guidelines:
Rest and Sleep: Get as much rest as possible. Sleep when the baby sleeps, and don’t hesitate to ask for help with household tasks.
Pain Management: Follow your healthcare provider’s recommendations for pain relief. This might include over-the-counter pain relievers or prescription medication.
Perineal Care: Keep the area clean and dry. Use a squirt bottle filled with warm water to cleanse after using the restroom, and pat gently with a clean cloth.
Ice Packs or Warm Compresses: Applying a cold pack wrapped in a clean cloth to the perineal area can help reduce swelling and discomfort. You can also use warm compresses to promote healing.
Hydration and Nutrition: Drink plenty of water and eat nutritious, balanced meals to aid in your recovery and energy levels.
Kegel Exercises: These help strengthen pelvic floor muscles, which can be weakened during childbirth. Your healthcare provider can guide you on when to start these exercises.
Avoid Heavy Lifting: Don’t lift anything heavy for a few weeks, as it can strain your healing muscles and tissues.
Stool Softeners or Fiber: To prevent constipation, consider using stool softeners or increasing your fiber intake. This can make bowel movements more comfortable.
Gentle Exercise: Once you get clearance from your healthcare provider, engage in light, low-impact activities like walking. This can help with circulation and mood.
Postpartum Check-ups: Attend your follow-up appointments with your healthcare provider to ensure that you’re healing properly.
Emotional Well-being: Pay attention to your mental health. If you’re feeling overwhelmed or experiencing symptoms of postpartum depression, seek support from your healthcare provider, family, or a mental health professional.
Breastfeeding Support (if applicable): If you’re breastfeeding, seek guidance from a lactation consultant or healthcare provider if you encounter any challenges.
In Conclusion,
Vaginal birth, also known as birth canal delivery, is a natural process with several advantages. It allows for a more rapid recovery compared to a cesarean section and promotes early bonding between mother and baby. It also carries a lower risk of surgical complications. However, it’s important to acknowledge that vaginal birth can be physically demanding, potentially resulting in perineal tearing or episiotomy.
Additionally, there may be a risk of certain complications, necessitating careful monitoring by healthcare professionals. Ultimately, the choice between vaginal birth and cesarean section should be made based on individual medical considerations and preferences, and it’s crucial for expectant mothers to receive comprehensive prenatal care and discuss their options with their healthcare provider.